Post-Caregiving Déjà Vu
Posted: June 11, 2021 Filed under: Aftermath of Caregiving, Assuming Caregiving Responsibilities, Caregiving Roles and Responsibilities, Emotional and Physical Challenges, Financial Considerations, Impact on Family Relationships | Tags: 24/7 Caregiving defined, Caregiving Commitments, Pamela Wilson, The Caring Generation Leave a comment
In regard to the June 2, 2021, Caring Generation Podcast—Taking Care of Family: Living for Someone Else—by Pamela Wilson–when I listened to this Podcast, I checked all of the following off as having had a significant impact in my own 24/7 caregiving experience. Supportive examples from What to do About Mama? are in blue.
24 7 Care For Elderly – The Caring Generation® – Pamela D Wilson
What does 24/7 care mean?
- The individual in need of care may be at risk of injury or other safety concerns if left alone for any time during a 24-hour period.
- The term 24/7 care is often first heard after an elderly parent is either hospitalized, or in a nursing home for rehabilitation after a serious injury or health issue.
Mom nearly collapsed twice Monday night while I was helping her from the bathroom to the bedroom. I just could not physically handle her anymore. Normally I become highly focused when there is a problem to solve, but this time I felt at a loss about how to proceed. I called the doctor on his cell phone, and he instructed me to take her to the ER. He also said that my mother-in-law was probably moving beyond my ability to care for, and that we should consider placing her in a nursing home.
An Unremarkable and Imperfect Grandma, (my memoir) p. 414
Goal upon release:
- If a parent has been living alone at home, the individual’s goal or the family’s wish is usually for a return to independent living.
When Mom was discharged, she returned to the retirement facility. The day after Thanksgiving she fell in her apartment, resulting in another trip to the emergency room. She had broken her pelvis again, this time in two places on the other side, which resulted in another hospital stay and another nursing home admission for rehab. Mom was discharged after two months and returned once again to her retirement home in early 2007. However, this time David and I informed Mom and his siblings that we were not going to repeat this process if she was injured and debilitated once more; something had to be done to put an end to this vicious cycle.
What to Do about Mama? p. 11
- Parents often deny they need “help” because the term can have a negative connotation when viewed as meaning “incapable of self-care”.

- The ability to return to independence can be vague in terms of time and ability level.
Caregivers sometimes begin by providing support in such areas as yard work or home repairs, followed by assistance with IADLs: telephone communication, housekeeping, laundry, food preparation, transportation, and managing medications and finances. Perhaps a greater sense of dependence involves the need for support with ADLs: bathing, dressing, grooming, ambulating, transferring, toileting, and feeding. The list of caregiving tasks grows and grows; the specifics are customized to each individual situation. When I was no longer able to care for my mother-in-law because of my knee replacement surgery, I wrote a job description for our nephew, which, in addition to the above-listed responsibilities, included the following tasks:
*Maintain an updated medical history to take to all doctor appointments
What to Do about Mama? p. 162
*Maintain hearing aids; help to put them in
*Manage oxygen
*Perform wound care
*Order medications, medical supplies, and equipment
*Order incontinence products
*Take to hair and nail appointments
*Provide opportunity for recreational activity
*Schedule and direct help–aids and hospice personnel
A serious talk is needed to determine:
- What level of independence necessary to return home?
- What efforts will need to be made?
- How much involvement and commitment will be required of caregivers?
- Will your parent commit to following doctor’s orders? Will he/she go above and beyond to establish habits that support better health and more physical activity?
We talked to Mom, and she seemed to understand that I could not continue to be her caregiver. The burden of caregiving – which now included hands-on assistance with walking and transferring, maintaining the oxygen and carrying the bottles, pushing the wheelchair and lifting it in and out of the car, cleaning up after episodes of incontinence, and, most significantly, wound care of her arms and lower extremities – was just more than I could handle in my current physical condition.
What to Do about Mama? p. 434
Options to be explored:
- Paid in-home caregivers
When the Aging care manager outlined the specifics of the waiver program’s “Services My Way” plan, I was floored. It provided more than I had dreamed in my wildest imagination: A 24/7 service provider; expensive equipment, such as an electric Hoyer lift, a customized wheelchair, and a combination shower wheelchair-commode; and environmental modifications, including ramps, laminate flooring, and a handicapped-accessible bathroom modification with a wheel-in shower chair.
What to Do about Mama? p. 314
- Moving to a care community.
I accepted more responsibility as my parents’ conditions worsened. Eventually, my mom convinced my dad they should move to my city to end the last-minute emergency flights for me and allow me to keep closer tabs on their situation, including help arrangements. I chose a continuing care retirement community (CCRC) near my house, and it was the best decision for them and for me. My mother called the shots on the move, and of course, I agreed. Moving them to my hometown was the biggest change in my caregiving situation, and it certainly did ratchet up my involvement and time commitment.
What to Do About Mama? From Marianne’s Story p. 98
- Relying on family caregiving
Boundaries to be set:
- As the caregiver, what level of time or money you can you commit?
Secondly, I was a caregiver for seven years. During the time I worked at Aging, my mother-in-law moved from Florida to our city in Pennsylvania. She resided in a supportive independent living retirement facility. After living there for two years, she began to have falls, which required a cycle of emergency room visits, hospitalizations, and extensive rehabilitation. The “solution” to the problem was for me to quit my job so that my mother-in-law could move into our home with me as her full-time caregiver.
What to Do about Mama? p. 2
If care becomes permanent, what will be the next steps taken to meet increasing needs?
Because BGM had quit her job, and her income was essential to meeting the mortgage, she and her husband became financially dependent on his mother. That left them little recourse when the burden became too much for BGM to physically handle.
What to Do about Mama? p. 252
A problem to avoid:
- Caregivers contributing to the situation by becoming indispensable. Be aware that each hospitalization or nursing home stay opens up another point for decision-making since escalating needs require new approaches.
She made comments such as, “You’re evicting an eighty-nine-year-old woman!” and “I feel protected here.”
“I understand that you are that you are apprehensive of change and what it will be like for you living at Shelley’s. I say with confidence that Shelley is very capable and resourceful and will see that you are well-cared for. And after all, she is your daughter.”
What to Do about Mama? pp, 32 & 35
A principal to follow:
- Establishing equal participation in care. This is essential so that that caregiver does not become responsible for taking on total responsibility for a 24/7 care situation.
Develop a “contract of expectations and commitments that everyone understands, agrees to, and signs off on.
What to Do about Mama? p. 255

How many of you have been inundated with a show of hands?
The Aftermath of Caregiving
Posted: January 1, 2021 Filed under: Aftermath of Caregiving | Tags: end of caregiving, Harriet Hodgson, mixed emotions, Moving forward, The Caregiver Space Leave a commentLife after caregiving can be full of surprises. What I mean is, our reactions and feelings can be so different from what we may have expected. In the 2nd Edition of What to Do about Mama? I added a new chapter that spoke directly to the matter of life after caregiving.
The Caregiver Space article, December 7, 2020, “Moving Forward After Caregiving Ends” by Harriet Hodgson, focuses on the same topic.
For over 23 years, Harriet cared for three generations of family members in one form or another. Saying caregiving was “woven into every thread” of her life, she explains why she, as a health and wellness author, changed the focus of her writing to books for family caregivers.
Harriet also explains that she writes to learn and figure things out. In her article she compiles a list showing her thought process after her beloved husband died, November 2020. See: Moving Forward After Caregiving Ends | The Caregiver Space
After completing her exercise, Harriet sums it up like this: “When caregiving ends, we need to give ourselves time to get our bearings. We need to give ourselves time to recover from shock. We need to give ourselves time to identify our feelings. We need to give ourselves time to plan a new life. We need to give ourselves time for renewal. Most importantly, we need to believe in ourselves. Love will guide us and lead the way.”
Because I have often noted that when caregiving responsibilities end there is a common reaction of, “What now?” So, in preparation for writing a new chapter for the 2nd Edition of What to Do about Mama? I asked the following question of post-caregivers: “When your caregiving ended, what was your initial reaction; and what did you do to move on?” Here are some of the responses:
I found myself with a void to fill—a process that just started to evolve naturally. I began to look for things to do, and now I look back and am amazed that I was able to spend so much time with my dad. Amelia p. 276
Initially, after my mother passed away and my caregiving ended, I felt an overwhelming amount of emotion and logistics to sort through. Once that was settled, though, it was just one day at a time, going through the motions until eventually the motions didn’t feel like such an effort anymore. It is fortunate, I suppose, that as a parent of young children, there is not much choice about moving on. Jenna p. 280
When my mother passed away, I felt lost. It was like losing a child. I felt unneeded—like I had lost a lot of my importance and purpose in life. Caregiving took up a large percent of my day, and suddenly having so much time on my hands was a difficult adjustment for me. Ellen p. 282
Due to therapy, I started writing on a daily basis, which is a major help. I am happy to have had productions of my work all over the world. My most recent work is about, you guessed it, caregiving! Jeanette p. 285
Surprisingly, I have moved on with great peace. I know that I did my best, given the circumstances. June p. 286
At first, I was relieved her suffering was over, and I had a lot less stress. That was short lived, though, as I quickly missed the intimacy of caring for her. I missed her terribly. I started a support group for brain cancer patients and caregivers. I named it after and dedicated it to my wife. Curt p. 287
When she passed, I felt guilt that maybe I hadn’t done enough; that I hadn’t given her enough hugs and reassurances; that I could have helped her more. Though I was relieved on one level, I had a lot more haunting thoughts going through my head over her death. Judene p. 288
Post-caregiving, I found the best help in hospice counseling. After Dad passed away, my husband and I had to recreate a social life. It’s certainly an adjustment to have so much free time. It’s a version of empty nest syndrome, but this time with the added ingredient of grief. My advice? Get out and enjoy your new-found freedom. Marianne p. 290
My faith, great friends, and excellent hospice counselors brought me out after almost ten years of intense caregiving, with my mind and spirit intact. I have begun Life: Part II, with great thankfulness for God’s sustaining grace, past, present, and future. I fill my time now with friends, my children and grandchildren, volunteer work, and helping other people. I feel well-adjusted, whole, and happy. (So, there is life after caregiving, if you can survive it.) Katrina p. 290
When my caregiving ended, I sadly felt a sense of relief—despite the fact that I know I am now all alone. I like to think that now (in the afterlife) my mother or maybe my father or someone, just feels that this is Joanna’s time for Joanna. Who knows? I’m not questioning the how or the why. I’m just enjoying the journey! Joanna 292 & 294
What to Do about Mama? pp. 276-294

More about Denial
Posted: March 23, 2020 Filed under: Aftermath of Caregiving, Emotional and Physical Challenges, Miscellaneous | Tags: becoming care receivers, changing roles/changing the guard/passing the torch, crisis situation, denial, experts and dealing with reality, facing reality 1 CommentAnother day has come, and I want to continue the discussion about denial, which is currently having a significant impact on some individuals in my own family whom I dearly love.
In exploring caregiving websites, I came across the following: Caregiving Made Easy http://www.caregivingmadeeasy.com See also: https://caregivingmadeeasy.blogspot.com/2010/07/welcome-to-care-giving-made-easy.html
It looks like a really good website, but I am stuck on its name. It’s a pet peeve of mine when I hear the message, “Just follow these steps and caregiving will be easy.” Education certainly helps, but when caregivers are told that following good advice will make it easy, it elicits a sense of failure when it is not. Even experts who find themselves in the role of caregiver find that caregiving is never easy.
As a matter of fact, being an expert can even create additional frustration. As an expert, you have high expectations of yourself. This only increases the pressure because you feel you should “know it all.”
“After all, who better to understand what was happening than I? I say this factiously, because I am a palliative/hospice nurse and a former director of nursing for an assisted-living community with a dementia unit. However, none of that helped me deal with the reality of my mother’s condition. I soon learned how inept I really was at managing her care. The result was that it took a crisis for me to be able to step in and take charge of moving my mom to a safer and more manageable environment.”
What to Do about Mama? June’s Story, page 142
In my family, there are now-senior members who are historically the experts. They are the go-to people for all questions related to medical issues and well-being. Accustomed to that role, they have not transitioned easily to accepting that they have become the folks in need. It has taken the CRISIS SITUATION to provoke them into doing what needs to be done. And despite having a very-competent next generation to help, they all need to learn how to navigate the changing of the guard—that process when parents relinquish control and children accept that their parents, who they always relied upon, are now the one one’s in need.
Here is the cold truth for my generation. We are next up at bat—not just as caregivers—but as care receivers. Most of us find that concept hard to accept, and it appears that we are in denial that the time is coming (or has arrived) for us to pass the torch.
But maybe the denial is being generated by more fundamental causes because we:
- value our independence and do not feel ready to give it up—even gradually;
- are self-conscious that it’s difficult to do things that were once easy;
- are uncomfortable with the idea that we cannot be depended upon as we once were;
- are afraid to lose our abilities to do such things that are now unsafe, such as driving or climbing ladders;
- lose once-familiar personality traits when depression makes us sad and saps our joy;
- withdraw and become socially isolated—feeling powerless that we can’t change what is happening;
- lose our core identity—our sense of self.
What to Do about Mama? isn’t a book by “experts,” but by regular people in the trenches. It may just resonate with you.
Thoughts about Denial
Posted: March 16, 2020 Filed under: Aftermath of Caregiving, Emotional and Physical Challenges, Financial Considerations, Impact on Family Relationships, Miscellaneous | Tags: attitudes about caregiving, avoiding caregiving, avoiding-crisis-mode, caregiving denial, denial, Information folders for family caregivers, proactivity and preparation for caregiving, procrastination and caregiving, viscous cycle of caregiving 2 CommentsI asked on my Home Page: Did you ever have a major life experience that made you say (or even just think), “I should write a book”? Well, I did. The Caregiving Experience. I kept a journal; I saved e-mails written to family; I had a veritable glut of relevant information and experience. So, what did I do with all this stuff? I wrote What to Do about Mama? The book was released November 2013, and within a couple of years I was thinking:
- Young people don’t think they need it yet.
- Caregivers are too darn busy.
- Post-caregivers just want to “put it all behind them.”
Believe me, I get it. But these attitudes are a core reason for why caregiving becomes one big viscous cycle. It usually takes a crisis to pull us out of the procrastination, avoidance, and denial mode. I want to tell you—that just ain’t no fun.
The 2nd edition of What to Do about Mama? has now been released. There’s a new chapter, The Aftermath of Caregiving, which deals with a number of these issues.
There are many steps you can take to be proactive about preparing for future caregiving needs. Many are discussed in the book. Here is just one:



- The folder has the relevant information our children (or surviving spouse) will need.
- Table of Contents: Financial (accounts, expenses, insurance, taxes and payments; Legal (information and paperwork); Property Maintenance (home and vehicles); Medical Information (insurance, medical history, wishes and preferences for end-of-life care); Other (information to access accounts, an inventory of belongings with our children’s and grandchildren’s preferences noted).
- The Conversation Project is a conversation starter, but it also contains our values, as well as our preferences for life-decisions and care. It is in the medical section.
- Our will and directives are also completed, but are in a separate file.
Denial of Caregiving:
Three articles of interest.
Daily Caregiving: 3 Ways to Deal with Family in Denial About Seniors Needing Help
https://www.dailycaring.com/3-ways-to-deal-with-family-in-denial-about-seniors-needing-help/
According to the Mayo Clinic, “Denial is a coping mechanism that gives you time to adjust to distressing situations.”
Why would someone be in denial?
- Asking someone to change how they see your older adult threatens their whole world. That’s usually why people fall back on denial.
- It’s safe and comfortable to pretend that everything is fine and nothing is changing.
- For some, denial is a subconscious way to ignore the fact that their parent or spouse is declining. For others, it’s a way to avoid taking on caregiving responsibilities.
A Place for Mom: 13 Dangers of Caregiver Denial
https://www.aplaceformom.com/blog/9-28-15-dangers-of-caregiver-denial/
Denial is a normal human emotion. No one wants to confront diseases such as Alzheimer’s for which there is currently no cure. Caregiver denial presents dangers that puts the caregiver at risk, as well as the care receiver. Elizabeth Lonseth, whose parents and parents-in-law were all diagnosed with memory impairment, is the author of “A Gradual Disappearance”. Elizabeth is up-front that it doesn’t matter how many times you’ve been through the caregiving experience—it never gets easy. But a little education helps, and the article presents some good pointers and survival tips to keep in mind.
- 7 Dangers of Denial for the Patient
- 6 Dangers of Denial for Family Members
Our Aging Parents: Are Your Elderly Parents In Denial? By Mike Gamble
https://ouragingparents.net/elderly-parent-denial
This article questions whether what appears to be denial is really triggered by underlying causes, and that progress depends on understanding those causes.
- Pride — Fiercely independent, they simply don’t want to admit they can no longer do many of the things needed to live independently.
- Embarrassment — They are uncomfortably self-conscious because they can’t do things they used to do with ease.
- Ashamed — They are afraid of disappointing friends, family members and other people they admire and love because they are no longer capable of living independently.
- Fearful — They are afraid of losing their independence and/or their ability to function independently. Such as giving up driving
- Depressed — They look sad, talk less, never smile, are joyless, believe they are a burden.
- Powerless — They feel helpless — like they no longer have the power or ability to act to change their circumstances. They withdraw, become socially isolated.
- Core Identity — There’s nothing that leaves you feeling more powerless than losing your core identity.
This last list is really hitting home for me right now. I’ll save that discussion for another day.
Barb Matthews
The “We don’t need it yet” phenomenon
Posted: February 22, 2020 Filed under: Aftermath of Caregiving, Emotional and Physical Challenges, Impact on Family Relationships | Tags: avoiding-crisis-mode, conversation project, denial, difficult conversations 2 Comments
For me, writing a book is an all-consuming process. After What to Do about Mama? was published in November 2013, I tended to refer to “my book” a lot in family conversations. My three adult children, who I encouraged to read the book, tended to tire of the topic. As my oldest daughter explained, “We don’t need it yet.”
There are four sets of grandparents in our family group. But, by the end of 2018, two of my “counterpart” grandmas had passed away. Life comes at you fast. Suddenly the kids realized they did indeed need the book. But at that point, as is typical in these situations, who had the time?
An article on caring.com, “Starting-the-conversation” discusses how to broach difficult subjects with aging parents. https://www.caring.com/caregivers/starting-the-conversation/
But how do you broach difficult subjects with your children, or maybe more
specifically, your children-in-law? My son-in-law’s (SIL) parents were both diagnosed with cancer in the span of a year. Seeing a need, and knowing that I had some useful information, I simply offered SIL a printout of The Conversation Project: https://www.theconversationproject.org/
Glancing at it, but not actually reading it, he noted language that brought
to mind difficult topics he did not want to acknowledge. In his denial, he charged me with being “insensitive” and he did not consider using the resource.
Clearly, my approach did not work well; unfortunately, it caused a shift in
our relationship; and sadly, within his family, some important information was not shared.
It is my impression that when it comes to caregiving, people often fall into
one of three categories:
- Pre-caregiving—“We don’t need it yet.”
- Current caregiving—“Who has the time?”
- Post-caregiving—“I just want to put it all behind me.”
The result? The cycle of “caregiving-in-crisis” continues.
Check out one of my previous posts on this topic: https://bgmatthewsblog.wordpress.com/2014/02/11/the-conversation-project/
What to Do about Mama? Expectations and Realities of Caregiving
Posted: February 16, 2020 Filed under: Aftermath of Caregiving, Miscellaneous | Tags: "What to Do about Mama?", 2nd Edition Leave a comment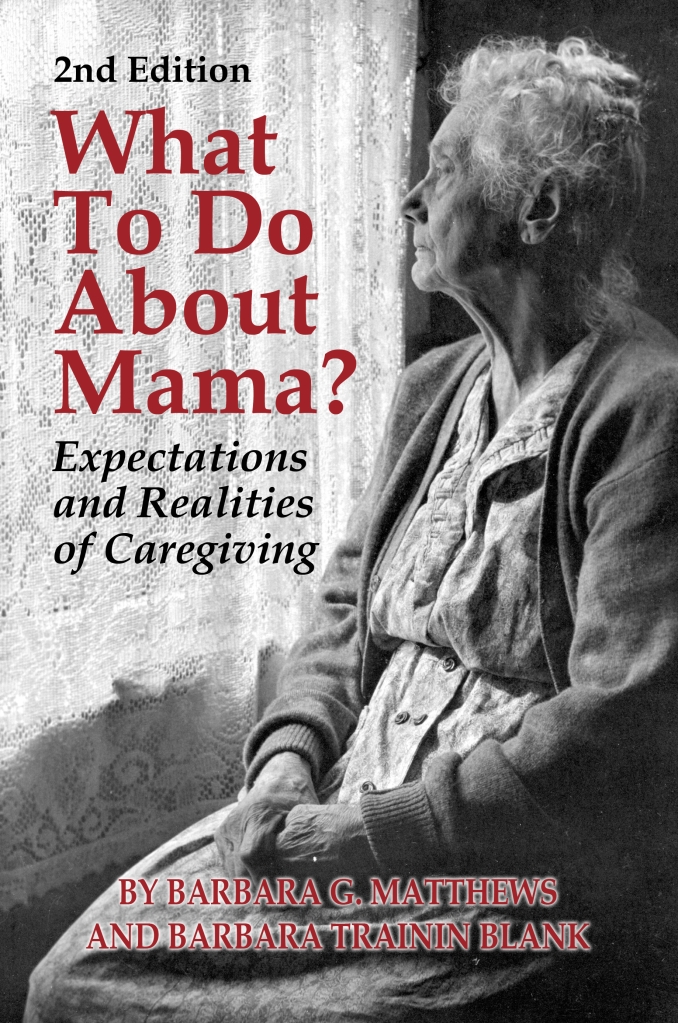
The hiatus has ended. Stay tuned.
What to look for in the 2nd edition:
- New subtitle
- New cover
- New, easier-to-use formatting
- An Index
- A new chapter: The Aftermath of Caregiving



